Does your significant other complain that your snoring wakes them up during the night or keeps them from getting to sleep in the first place? Do they poke you, waking you up because sometimes they're afraid you stopped breathing? If so, you may have a condition called obstructive sleep apnea. When you have sleep apnea, the flow of air to your lungs pauses or decreases while you sleep.
This happens because your airway has become narrow or blocked. While you sleep, all of the muscles in your body become more relaxed, including the muscles that help keep your airway open, allowing air to flow freely to your lungs. Normally, your upper throat still remains open enough during sleep to let air easily pass by. When the muscles in their upper throat relax during sleep, their breathing can stop, often for more than 10 seconds. Often you're not aware that you stopped breathing during sleep. But you may wake up not-refreshed, and feel drowsy and tired during the day.
If you have this condition, your doctor will perform a physical exam, carefully checking your mouth, neck, and throat. You may take a survey that asks a series of questions about daytime sleepiness, sleep quality, and bedtime habits. If your doctor suspects you do have sleep apnea, you make take a polysomnogram, a sleep study that monitors you while you sleep.
Once your doctor diagnoses sleep apnea, treatment will focus on keeping your airway open so that you breathe better while you sleep. You can avoid alcohol or sedatives, and not just at bedtime, avoid sleeping on your back, and try to lose weight if you need to. And, exercise can help, even in the absence of weight loss.
Your doctor can also prescribe a positive airway pressure using a machine, with a tight-fitting face mask, that pumps slightly pressurized air into your mouth during your breathing cycle. Some people need to wear dental devices that keep their jaw forward during sleep. If lifestyle changes and devices don't help, surgery may be an option. Untreated sleep apnea, however, may lead to or worsen heart disease.
Most people with sleep apnea who get treatment have less anxiety and depression than they did before. Naturally, having less daytime sleepiness can lower your risk for accidents at work, while you drive and give you more energy throughout the day. First, although this represents the largest reported cohort of patients with DS undergoing T&A, the absolute number of patients was still relatively small. If there was a longer window for the PSG to be obtained, the OAHI may no longer be representative of their preoperative or postoperative OAHI.
Because children with mild OSA may be less likely to have a postoperative PSG, this possibly biased the results. One could assume that those children with mild OSA and persistent symptoms would be more likely to have a postoperative PSG. For an asymptomatic child postoperatively who had only mild OSA preoperatively, the parents may not see the benefit nor want to pay out of pocket for a repeat study. The physician may also not see the necessity of testing an asymptomatic child because they would not be recommending any intervention if the OSA was still mild. Second, the number of African-American children in the cohort is small, potentially influencing ethnicity's role on surgical success.
Because the 2015 guidelines relax the scoring criteria for hypopneas, outcomes studies that include children from 2015 may have less favorable results. A major limitation of this study is that it was retrospective and uncontrolled in nature. A prospective trial with universal postoperative sleep studies would provide a more accurate estimate of surgical efficacy. Discussion/General InformationTonsillectomy is one of the most common surgical procedures in the United States, with more than 530,000 procedures performed annually in children younger than 15 years of age.
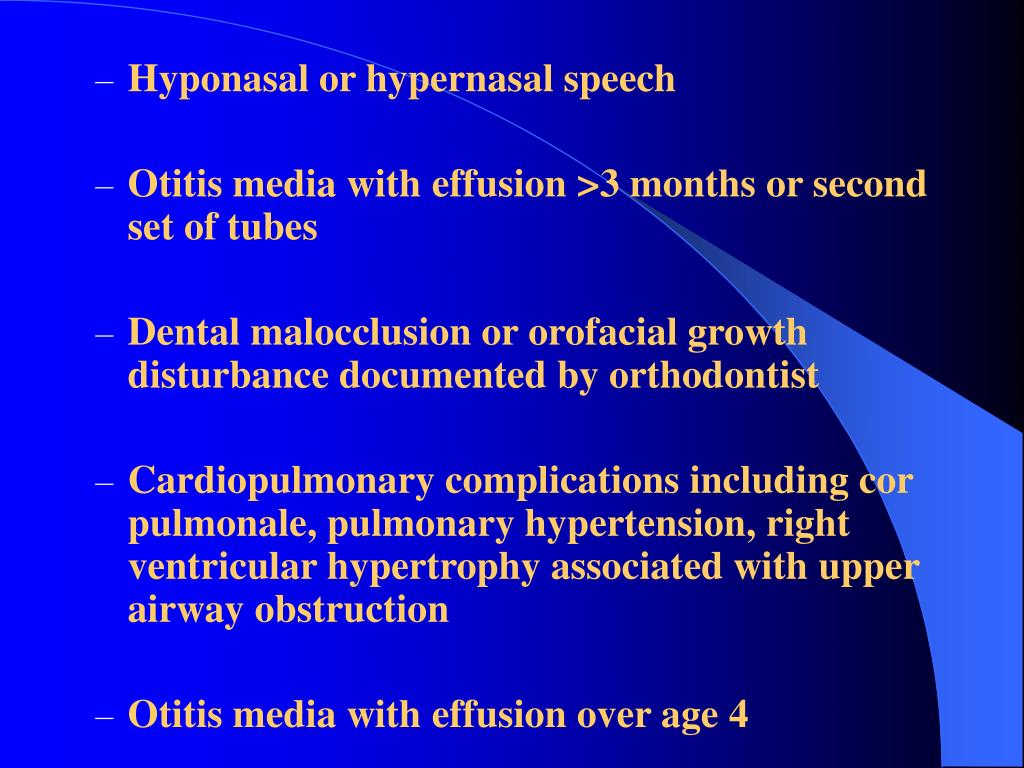
Depending on the context in which it is used, it may indicate tonsillectomy with adenoidectomy, especially in relation to sleep-disordered breathing . Indications for surgery include recurrent throat infections and SDB, both of which can substantially affect child health status and quality of life. Although there are benefits of tonsillectomy, complications of surgery may include throat pain, postoperative nausea and vomiting, delayed feeding, voice changes, post-tonsillectomy hemorrhage , and rarely death. Further interventions may be needed, both surgical and medical. All of these studies illustrate the need for post-operative evaluation of patients with Down syndrome for residual sleep apnea after T&A surgery with a post-operative sleep study or polysomnogram.
Because of the higher rate of respiratory complications after removal of the tonsils and adenoids in individuals with Down syndrome, overnight observation in the hospital after this surgery is also recommended. For adults with obstructive sleep apnea, the standard treatment is positive airway pressure therapy . Surgery is reserved for patients who are unable to tolerate or benefit from positive airway pressure therapy. For children, adenoidectomy and/or tonsillectomy for sleep apnea is the standard treatment.
Positive airway pressure therapy is not an ideal treatment for most children. This is due to concerns over effects on facial growth and difficulty that children may have with tolerating it through the night. It is reassuring that surgical outcomes in children–while by no means perfect–are relatively good, especially when the tonsils or adenoids are enlarged and when the child is not considered substantially overweight.
Tonsillectomy has been demonstrated to be an effective treatment tool for OSA in both children and adults. While there are hundreds of articles published regarding tonsillectomy, it is difficult to find systematic reviews of tonsillectomy alone, especially for pediatric patients. Tonsillectomy and adenoidectomy are most often performed simultaneously as the primary treatment for OSA in children. Pediatric success and cure is variable based on clinical factors such as tonsil size, palate position, craniofacial abnormalities, comorbid syndromes, and obesity. The literature supports adenotonsillectomy as the first treatment option for low risk as well as children with Down syndrome and obesity.
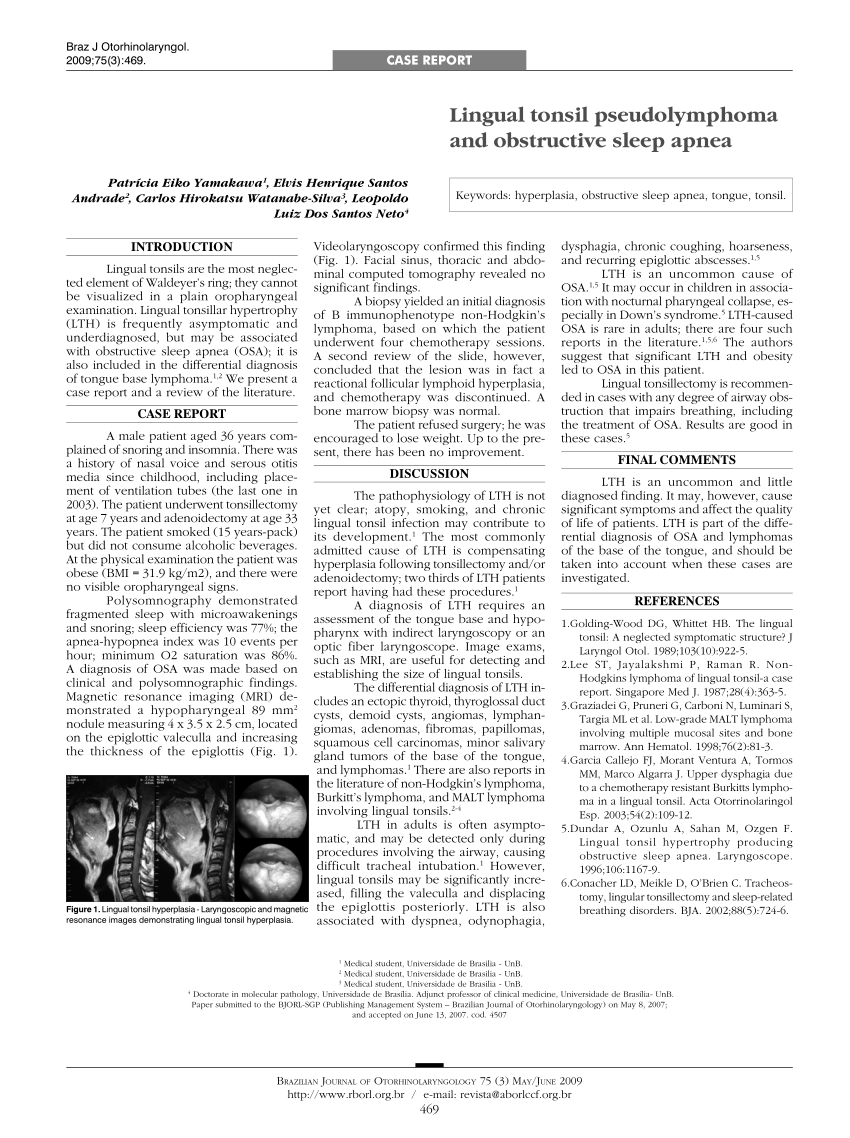
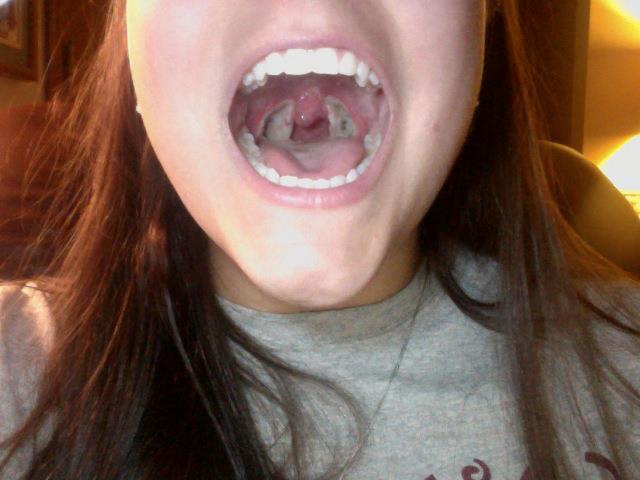
It is essential, however, when counseling families to mention other treatment options and likelihood for residual disease. Tonsillotomy may also be a surgical consideration to decrease the risk of bleeding and has demonstrated efficacy. As part of the exam, your doctor will check your mouth, nose, and throat to determine areas of obstruction. For example, a deviated spetum, large turbinates, enlarged tonsils, a long or thick uvula , a floppy soft palate or a large base of tongue. Your doctor may order a sleep recording if your symptoms are severe enough based on your history, exam and questionnaire results to grade your sleep apnea into mild, moderate or severe types.
SDB is the second most common indication for tonsillectomy in children and is characterized by disturbances in breathing pattern or efficacy during sleep. Unfortunately, there is no widely accepted standard for the diagnosis of SDB. However, it is recognized that SDB may involve snoring, mouth breathing, and pauses in breathing . Daytime symptoms associated with SDB may include excessive sleepiness, inattention, poor concentration, aggression, depression, hyperactivity, and wetting the bed. A wide array of obstructive disorders may result in SDB, ranging in severity from simple snoring to obstructive sleep apnea.
The most common cause of SDB in children is tonsillar hypertrophy, which is an abnormal enlargement of the tonsils. This may be due to chronic infection or excess tissue growth. Diagnosis of SDB may be based on an individual's medical history, physical examination, audio/video taping, pulse oximetry, or limited or full-night polysomnogram, also known as a sleep test.
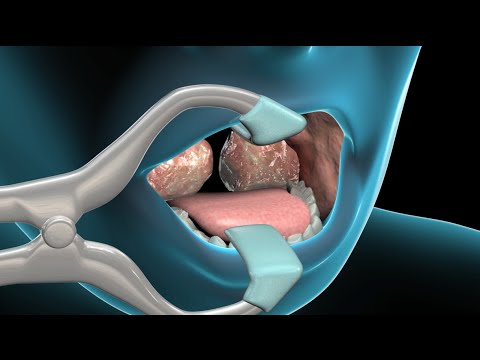
History and physical examination are the most common initial methods for diagnosis. Treatment may involve antibiotics to address underlying infection, but if such treatment fails or is not indicated, tonsillectomy may be warranted. The treatment for obstructive sleep apnea is based on the cause. Since enlarged tonsils and adenoids are the most common cause of airway blockage in children, the treatment is surgery and removal of the tonsils and/or adenoids .
Your child's otolaryngologist will discuss the treatment options, risks, and benefits with you. Depending on the health of the child, surgery may be performed on an outpatient basis. This procedure, and other types of soft palate surgery, targets the back of your mouth. It involves removing and repositioning excess tissue in the throat to make the airway wider. The surgeon can trim down your soft palate and uvula, remove your tonsils, and reposition some of the muscles of the soft palate. UPPP and other soft palate procedures are the most common type of surgery for sleep apnea.
But UPPP alone is unlikely to cure moderate to severe sleep apnea. It may be combined with surgeries that target other sites in the upper airway. We are in the midst of a major change in rethinking sleep apnea surgery–for all parties involved. The goal is developing a tailored approach to sleep apnea treatment with an approach that is often called personalized medicine. I see many young adults with markedly enlarged tonsils who are struggling with positive airway pressure therapy, including many with mild sleep apnea who are not overweight.
For these patients, I think it is very reasonable to think about surgery as a first-line option instead of being on positive airway pressure for the rest of their life. These patients have a greater than 90% chance of clearing up their sleep apnea with tonsillectomy alone. Not every one of them will want to have surgery, but this should be part of the discussion because the results will be so good, based on everything we know about sleep apnea surgery outcomes. The December 2016 issue of the medical journal The Laryngoscope included an interesting study examining this question.
Twenty-nine adults with markedly enlarged tonsils (size 3+ or 4+ on the Friedman scale), obstructive sleep apnea, and no substantial obesity (body mass index below 32 kg/meters squared) underwent tonsillectomy alone. One patient was lost to follow up, but the rest of the patients had sleep studies before and then 6 months after surgery. Impressively, the average apnea-hypopnea index decreased from 40 to 7 events per hour after undergoing tonsillectomy for sleep apnea, with only 2 patients having anything worse than mild sleep apnea. There were also substantial improvement in the score on the Epworth Sleepiness Scale score that measures daytime sleepiness . In children, the most common cause of obstructive sleep apnea is enlarged tonsils and adenoids in the upper airway. Large adenoids may completely block the nasal passages and make breathing through the nose difficult or impossible.
As in adults, the gold standard diagnostic test for OSA in children is polysomnography , which physiologically tests sleep architecture and efficiency. Treatment involves alleviating the inciting upper airway soft tissue obstruction or collapse. One method of primary treatment is continuous positive airway pressure .
CPAP compliance is highly variable in children.6–10 Other approaches include weight loss in overweight children, oral appliances, and allergy or antiinflammatory medications. However, because the most common culprit in children is tonsillar hypertrophy-related oropharyngeal obstruction, tonsillectomy is often used to establish an adequate airway. In recent years, intracapsular tonsillotomy has emerged as an alternative surgical option to total tonsillectomy for OSA in children. During this in-office procedure a rim of soft palate containing the uvula is removed using the laser.
In the past the laser used was the CO2 laser which was associated with significant pain for up to 2 weeks following the procedure. However our physicians now utilize the cold laser or radiofrequency energy to obtain the same result with significantly less discomfort which consists of a mild to moderate sore throat for approximately one week. Most patients state that the discomfort is manageable and after hours they can resume normal activities, although a soft diet is recommended for one week. In carefully selected patients this procedure as a stand alone procedure or in combination with the pillar implant procedure can provide tremendous improvement in snoring and sleep apnea symptoms. Call our surgeons serving the Los Angeles and Thousand Oaks areas to schedule a consultation to discuss if you are an appropriate candidate for this revolutionary procedure. Most children with sleep disordered breathing have enlarged tonsils and adenoids, and removing this tissue results in a cure of OSA in more than 90% of patients.
Snoring may persist after surgery, but if there is no more apnea, the snoring itself does not require any treatment. In some cases, however, there are other causes of SDB which will result in persistent OSA after surgery. These include obesity, a small jaw, a big tongue, a variety of congential skull abnormalities, or neurological problems causing poor muscle tone. The most frequent indication for tonsillectomy is recurrent throat infection. According to the AAO-HNS, a throat infection is defined as sore throat caused by viral or bacterial infection of the pharynx, palatine tonsils, or both, which may or may not be culture positive for group A streptococcus.
This includes strep throat infection and acute tonsillitis, pharyngitis, adenotonsillitis, or tonsillopharyngitis. The treatment methods used to address throat infections will depend upon the cause of the infection, but medications such as antibiotics and anti-inflammatory drugs to treat infection and alleviate symptoms are common. When an individual has frequent throat infections despite optimal treatment, the use of surgical interventions such as tonsillectomy may be warranted. Fiberoptic endoscopy must be performed systematically in association with one imaging test to determine the extent of soft tissue surgery needed, but the classic UPPP is not recommended in children. Studies have demonstrated long-term improved quality of life for these patients.
Newer data suggest that sleep apnea may negatively contribute to certain conditions such as attention deficit hyperactivity disorder and correction of the apnea leads to lower disease severity and reduced medication usage. The most critical aspect of early success is the complete removal of obstructing tissue. Because of this, the authors recommend visual inspection of the adenoid bed even if the technique to remove the adenoids was a blind one.
In patients whose symptoms return several months to years after the initial procedure, adenoid regrowth must be considered. An article by Emerick and Cunningham sheds light on a potentially overlooked cause of recurrent symptoms, hypertrophy of the tubal tonsils. Tubal tonsils, also known as Gerlach tonsils, are found beneath the mucosa in the region of the torus tubarius. Hypertrophy of this tissue has been shown to cause symptoms similar to those of adenoid hypertrophy. In this study, tubal tonsils were ablated using suction cautery.
Obstructive sleep apnea occurs when a child stops breathing during periods of sleep. The cessation of breathing usually occurs because of a blockage in the airway. Tonsils and adenoids may grow to be large relative to the size of a child's airway .
Inflamed and infected glands may grow to be larger than normal, thus causing more blockage. The enlarged tonsils and adenoids block the airway during sleep, for a period of time. The tonsils and adenoids are made of lymph tissue and are located at the back and to the sides of the throat. Removal of enlarged tonsils and adenoids is the first line surgical treatment. In individuals with Down syndrome, because of their midface hypoplasia and contracted nasopharynx, even mildly enlarged tonsil and adenoids may have a greater than expected effect in regards to airway obstruction. If the tonsils and adenoids do not appear enlarged, it has been suggested that a sleep study should be done to confirm that the individual does not have sleep apnea.
DISE is widely considered a useful tool with benefits for decision-making regarding upper airway surgery in patients with OSA.22 The correlation between the staging pattern of DISE and surgical outcomes was also investigated. All five patients with CCC benefited from the surgery, with a reduction observed in the AHI value, an increase of minimum SaO2 and an improvement in daytime sleepiness . However, three patients failed to satisfy the Sher criteria for surgical success. Residual collapse of the upper airway was indicated to be present in the nonresponders postoperatively. Notably, most of the other 17 patients without CCC presented good responses to UPsT with significant postoperative improvements in ESS and AHI value. Hence, UPsT was a potentially effective surgery for patients with OSA exhibiting complete APC and partial collapse in preoperative DISE.